
The digital health revolution has arrived on our shores. With it has come a wave of new technologies many offering promising solutions to some of the world’s most complex health related problems. From this we have seen mass enthusiasm for digital health products, resulting in a rapid expansion of the commercial marketplace. A great number of health technologies, including smartphones, online programs and smartwatches, are now offered direct to the consumer for minimal cost, at any time or place. And whilst many of these technologies might revolutionise the way we access and deliver healthcare, the lack of empirical evidence is striking (Grist et al., 2017, blogged here for the Mental Elf by Natalie Nelissen; Hollis et al., 2015; Hollis et al., 2019, blogged here by John Torous).
Over the past decade, we have seen an increase in the number of clinical trials providing evidence for the positive benefits of digital health interventions (DHIs; Ebert et al., 2018; Hollis et al., 2015). However, many of these studies are small and limited in what they can tell us about the real world. When research has looked at technology use in naturalistic settings, such as how much consumers use DHIs in the real world (Baumel, Muench, Edan, & Kane, 2019; Torous et al., 2017), we have been forced to confront a less promising reality. For example, mirroring the power log distribution observed in many clinical studies (see the image below), we find that usage of mental health mobile apps tends to drop rapidly over time (Torous, Nicholas, Larsen, Firth, & Christensen, 2018).
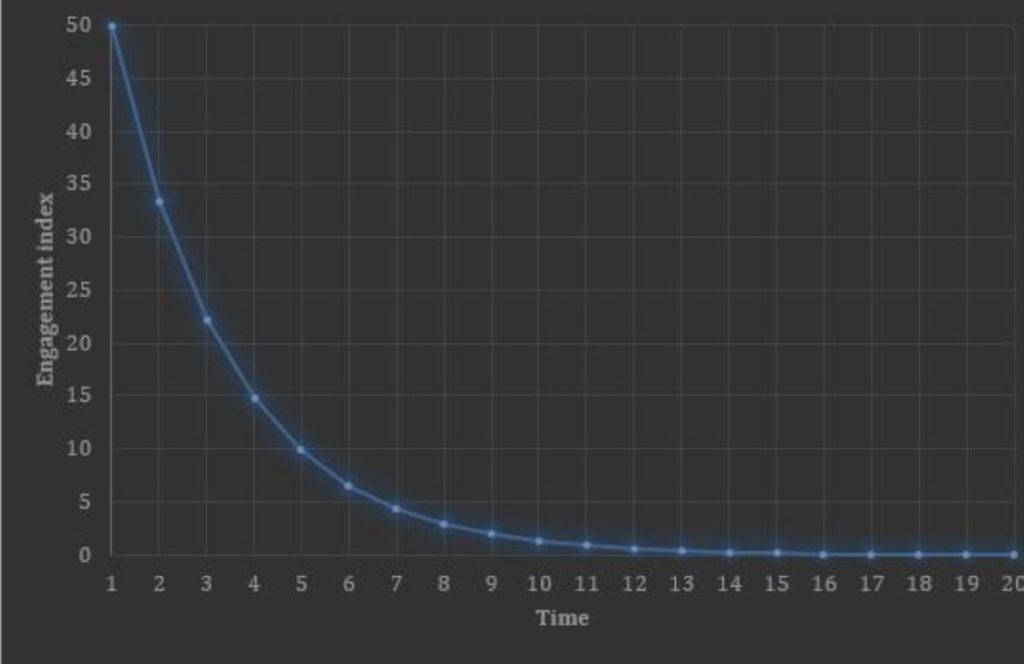
A typical distribution curve of engagement with digital health interventions over time: A high level of initial engagement which decreases exponentially over time.
This is troubling for a fairly obvious reason: for DHIs to be beneficial, people need to actually use them. They also need to work within the systems they were built for, which are different and more complex than the context of a clinical trial. As it turns out, this has been difficult to achieve, with implementation research highlighting that barriers to technology adoption are numerous and complex (Aref-Adib et al., 2018, blogged here for the Mental Elf by Mark Brown; Lattie et al., 2019; Mohr, Lyon, Lattie, Reddy, & Schueller, 2017). To address these issues, we need to change gears in health research and re-focus on what these barriers are and how to overcome them.
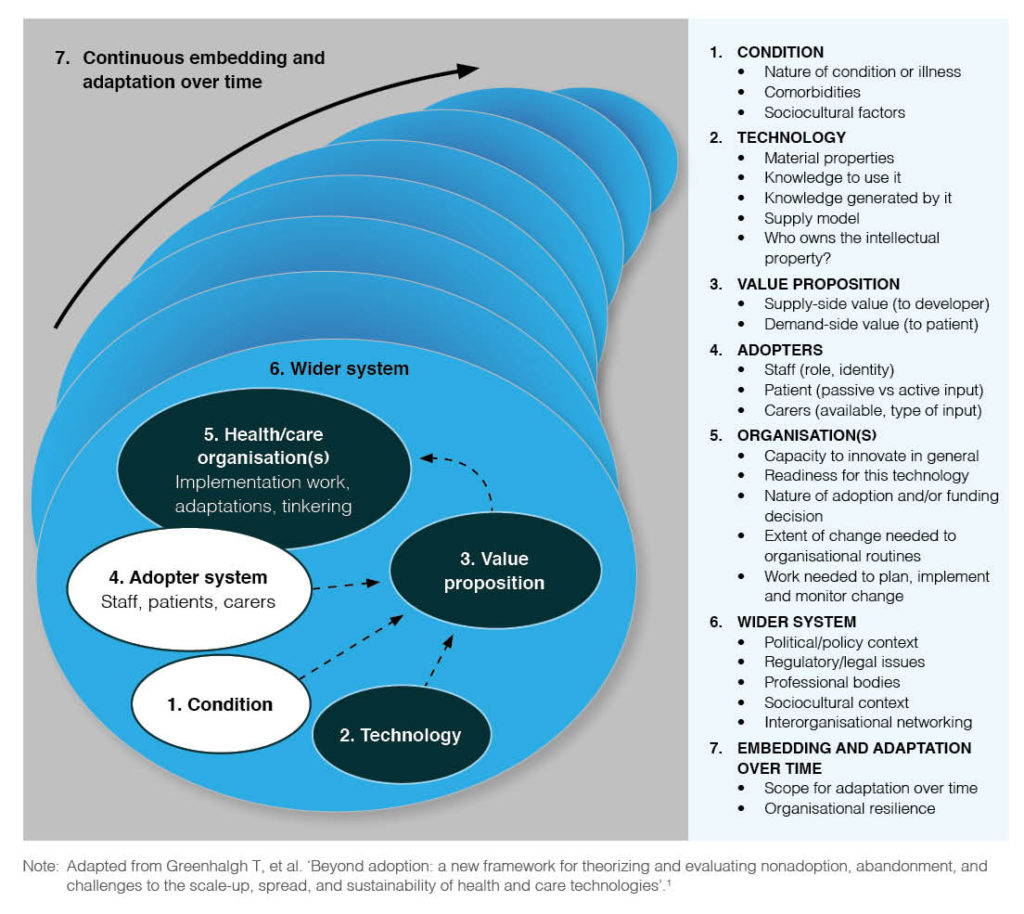
An article published in Public Health Research and Practice by Professor Trish Greenhalgh (2018) provides guidance on this complex topic. In this article, Greenhalgh outlines the NASSS framework (“Non-adoption, Abandonment, Scaleup, Spread and Sustainability”), highlighting five key problems underpinning the lack of technology adoption in healthcare and seven domains in which the complexity lies.
Methods
The author cites years of experience, case studies, qualitative research and a narrative systematic review (Greenhalgh et al., 2017), which informed the design of the NASSS framework. The research conducted by the author covers the evaluation and improvement of primary and secondary healthcare services, and the implementation of a range of health technologies across different health conditions.
Results
The article provides a concise overview of the framework, without going into explicit detail about the findings and experiences which informed its design. Five key problem areas loosely form the NASSS acronym:
“digital technologies are either Not Adopted or soon Abandoned by professionals and/or their patients and clients, or the technology-supported service succeeds as a small-scale demonstration project but fails to Scale up locally, Spread to other comparable settings or be Sustained over time.”
Seven domains of complexity relevant to what the author refers to as technology projects, are outlined. This term appears to refer to any project involving the design, testing and/or implementation of healthcare technologies. These seven domains are summarised in more detail than the problem areas, and are graphically represented in a clear and meaningful way within the article (see image below).
- Domain 1 refers to complexities in the illness or condition being studied, where a condition such as a sprained ankle has a clearer treatment pathway than a more complex condition such as drug dependency.
- Domain 2 refer to complexity in the features of the technology itself. A telephone call is relatively simple compared to a complex system designed to be used across organisations. Less complex technologies are reliable, affordable, and replaceable if needed.
- Domain 3 refers to the value proposition of the technology. Those designed with a clear justification and good return on investment are less complex than those without a clear business case or evidence to support their value.
- Domain 4 refers to the capacity or willingness of the end user to adopt the technology. The author states that this is the most common reason for the failure of health technologies. A less complex technology has users that are ready and willing to use it, whereas a more complex technology might involve users who lack capability or willingness, or perhaps choose not to use it for professional or personal reasons.
- Domain 5 is another area where health technologies often fail due to complexities within the organisation in which the technology is embedded. The complexity here is about whether the technology is a good fit for the system and takes into account relevant constraints, such as budgets and infrastructure.
- Domain 6 takes into account complexities within the broader systems and contexts that might limit the technology implementation. For example, a technology must adhere to the relevant professional guidelines and policies of the organisation.
- Domain 7 refers to the necessity of a technology to be flexible over time in order to adapt to changes within the system, i.e. how future proof it is. A complex technology in this case would be rigid in how it can be used and lacks the ability to be modified.
The capacity or willingness of the end user to adopt the technology is the most common reason for the failure of health technologies.
Conclusions
The article concludes by outlining how the NASSS framework can be applied to improving the success of technology projects, primarily focusing on the importance of minimising the seven domains of complexity. The authors refer to a tool they have created, which operationalises the domains into a series of questions that can help technology developers identify areas of complexity in their projects.
Managing and minimising complexity
Finally, ten principles are highlighted, which aim to help technology project teams to manage and minimise complexity. These are:
- Strengthen program leadership (which may be distributed across the project and across contributing disciplines)
- Codevelop an overall vision for the project, and maintain dialogue around that evolving vision
- Nurture key relationships between individuals and organisations
- Develop individuals, and encourage them to solve local problems creatively
- Make resources available for creative individuals and teams to use for generating solutions to local challenges
- Capture data on progress and feed it into ongoing deliberations
- Acknowledge and address the concerns of front-line staff
- Work with intended users to co-design technologies and the work routines they are intended to support, building in adaptability
- Control scope creep
- Address regulatory and policy barriers.

The authors outline how the NASSS framework can be applied to improve the success of technology projects.
Strengths and limitations
One critique is that the research underpinning the framework was not fully explored in this particular article, limiting understanding of its empirical basis. However, it is recognised that this piece was intended for a broader audience, particularly for policy and practice, making it easily digestible and practical in focus. The literature review and case studies are outlined in more detail in another article by the author and additional collaborators (Greenhalgh et al., 2017).
Another issue is that the framework is quite broad and it is difficult to know how to tackle these multiple intersecting layers of complexity, although this merely reflects reality and oversimplification would be inaccurate and unhelpful. The tool created by the researchers is useful in that it guides the identification of complexities and provides some advice for addressing them, but is rather lengthy and could perhaps be more specific in its guidance, potentially tailoring to different stakeholders and/or stages of technology development. It is somewhat difficult to conceptualise how the framework and tool will be used in practice, and the guidance principles are useful indicators but still quite broad.
Despite these issues, Greenhalgh (2018) provides a critical perspective at a point in time where it is really needed and the framework clearly captures the reality of the complexities underlying technology adoption.

The authors provide a much needed critical perspective of technology projects.
Implications for practice
This article is timely and relevant to a range of stakeholders in the field of digital technology and public health. It is important that those responsible for developing digital health technologies ensure they are readily implementable by addressing avoidable problems and complexities. This article communicates this caution in a clear and informative way, based on insights gained from a wealth of valuable research and experience, and provides a practical framework for recognising and tackling the problems before they arise.
In sum, our findings suggest that the overarching reason why technology projects in health and social care fail is multiple kinds of complexity occurring across multiple domains. Oversimplifying the challenge, or ignoring the uncertainties and interdependencies, won’t help. We need to shift gear and learn to run with complexity.

“Oversimplifying the challenge, or ignoring the uncertainties and interdependencies, won’t help. We need to shift gear and learn to run with complexity.”
Statement of interests
None to declare.
Links
Primary paper
Greenhalgh T. How to improve success of technology projects in health and social care. Public Health Res Pract. 2018;28(3):e2831815.
Other references
Baumel, A., Muench, F., Edan, S., & Kane, J. M. (2019). Objective User Engagement With Mental Health Apps: Systematic Search and Panel-Based Usage Analysis. Journal of medical Internet research, 21(9), e14567.
Ebert, D. D., Van Daele, T., Nordgreen, T., Karekla, M., Compare, A., Zarbo, C., . . . Jensen, K. L. (2018). Internet-and Mobile-Based Psychological Interventions: Applications, Efficacy, and Potential for Improving Mental Health. European Psychologist.
Greenhalgh, T., Wherton, J., Papoutsi, C., Lynch, J., Hughes, G., Hinder, S., . . . Shaw, S. (2017). Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. Journal of medical Internet research, 19(11), e367.
Hollis, C., Morriss, R., Martin, J., Amani, S., Cotton, R., Denis, M., & Lewis, S. (2015). Technological innovations in mental healthcare: harnessing the digital revolution. The British Journal of Psychiatry, 206(4), 263-265.
Hollis, C., Sampson, S., Simons, L., Davies, E. B., Churchill, R., Betton, V., . . . Gronlund, T. A. (2018). Identifying research priorities for digital technology in mental health care: results of the James Lind Alliance Priority Setting Partnership. The Lancet Psychiatry, 5(10), 845-854.
Lattie, E. G., Nicholas, J., Knapp, A. A., Skerl, J. J., Kaiser, S. M., & Mohr, D. C. (2019). Opportunities for and Tensions Surrounding the Use of Technology-Enabled Mental Health Services in Community Mental Health Care. Administration and Policy in Mental Health and Mental Health Services Research, 1-12.
Mohr, D. C., Lyon, A. R., Lattie, E. G., Reddy, M., & Schueller, S. M. (2017). Accelerating digital mental health research from early design and creation to successful implementation and sustainment. Journal of medical Internet research, 19(5).
Torous, J., Nicholas, J., Larsen, M. E., Firth, J., & Christensen, H. (2018). Clinical review of user engagement with mental health smartphone apps: evidence, theory and improvements. Evidence-based mental health, ebmental-2018-102891.
Torous, J., Staples, P., Slaters, L., Adams, J., Sandoval, L., Onnela, J., & Keshavan, M. (2017). Characterizing smartphone engagement for schizophrenia: results of a naturalist mobile health study. Clinical schizophrenia & related psychoses.
Photo credits
- Photo by Rodion Kutsaev on Unsplash
- Photo by Markus Spiske on Unsplash
- Photo by Gilles Lambert on Unsplash
- Photo by Adeolu Eletu on Unsplash
