
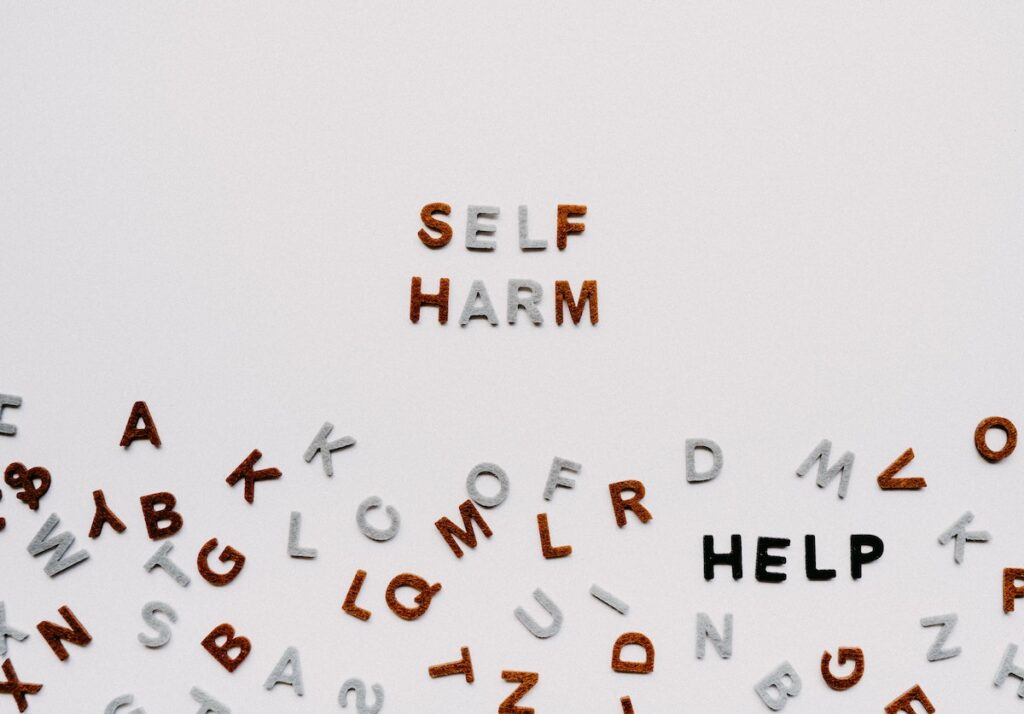
Rates of self-harm (both suicidal and non-suicidal) among young people are increasing in many countries, and self-harm is one of the strongest indicators of future suicide risk (Kamal et al, 2021). People with symptoms of psychotic and bipolar disorder are at particularly high risk (Clements et al, 2015; Haining et al, 2020). However, research to date has focused on the prospective relationship between these diagnoses and self-harm (i.e. risk of self-harm in people diagnosed with psychosis or bipolar disorder) with little attention paid to the possibility that the relationship may be bidirectional; that is, self-harm may also precede (or predict) the onset of psychosis or bipolar disorder.
A number of studies have reported high rates of self-harm before the onset of psychotic symptoms (Kelleher et al, 2013; Murphy et al, 2018), indicating that self-harm may be apparent before individuals seek help.
Many people who engage in self-harm do not present to clinical services (Gillies et al, 2018); but many do, and the rates of suicide after discharge from hospital are significantly higher than those in the general population (Forte et al, 2019). However, despite the elevated risk of suicide, and recommendations from governing or advisory bodies around the world (e.g., National Institute for Health and Care Excellence, 2013; Royal Australian and New Zealand College of Psychiatrists, 2009) many people who present do not receive a thorough mental health assessment, and many more are discharged without adequate follow-up care (Olfson et al, 2012).
With this in mind, in the present study, Bolhuis and colleagues (2021) sought to test the hypothesis that hospital presentation for self-harm would indicate risk of developing psychotic or bipolar disorders in a Finnish population study.

Young people with psychotic and bipolar disorders are at particularly high risk for self-harm and suicide.
Methods
This was a longitudinal, prospective register-based study based on data from the 1987 Finnish Birth Cohort study (Paananen et al, 2012), which included the entire population born in Finland in 1987. In the current study, individuals were followed-up until the end of December 2015 giving a maximum age of 28 years and a sample size of 59,476.
Data from several registers were linked for each individual via a unique personal identification code, which together enabled the authors to examine the prospective association between hospital presentation for self-harm and diagnosis of psychotic or bipolar disorder. Analyses were stratified by sex and secondary analysis examined risk in childhood and adolescence versus adulthood. Finally, time-to-event analyses examined the median length of time from self-harm presentation to a first diagnosis of psychotic or bipolar disorder.
Results
Of the 59,476 individuals included in the cohort, 481 had a lifetime history of hospital presentation for self-harm, with presentation being more common in females (261 vs. 220). Age at first presentation peaked at both 20 and 27 years and 36.8% of individuals presented more than once. 1,445 (2.4%) had a psychotic disorder diagnosis, 51 (3.5%) of which followed self-harm presentations to hospital. 770 (1.3%) received a diagnosis of bipolar disorder, and 43 (5.6%) followed hospital self-harm presentation. As per previous research, there was increased risk of self-harm presentations amongst individuals already diagnosed with psychotic or bipolar disorders.
Of those who presented to hospital with self-harm, but did not have a previous diagnosis, 12.8% went on to be diagnosed with psychosis and 9.4% with bipolar disorder by 28 years of age. Risk appeared to be higher amongst women, although the analysis suggests that this finding should be treated with caution.
Secondary analysis identified that younger age at first presentation corresponded to higher risk of subsequent diagnosis. Just over 10% of those who first presented with self-harm after the age of 21 went on to be diagnosed with psychotic or bipolar disorders, compared to 20.8% of those aged 18 to 21 years, and 29.1% of people who first presented before the age of 18.
There were no differences in risk between single versus multiple presentations.
The median time from first self-harm presentation to diagnosis was 0.75 years for psychosis and 1.79 years for bipolar disorder. The median time to a diagnosis of schizophrenia was longer at 3.07 years, but shorter for affective psychosis at 0.32 years.
This research suggests that self-harm presentations to hospital are a strong risk marker for a subsequent diagnosis of psychosis or bipolar disorder.
Conclusions
- Bolhuis and colleagues emphasise that the high risk of diagnosis was not related to self-harm per se, but rather to the clinical pathway, arguing that hospital presentations for self-harm represent a clear opportunity for the identification and subsequent treatment of psychosis and bipolar disorder.
- They also note that the period of time between presentation and diagnosis (over three years in the case of schizophrenia) represents an important “clinical window” during which appropriate treatment could have delayed, or even prevented, the onset of illness.

The authors of this research argue that hospital presentations for self-harm represent a clear opportunity for the identification and subsequent treatment of psychosis and bipolar disorder.
Strengths and limitations
Among the strengths of this study is the whole population approach, removing issues such as selection bias, and the enviable data linkage from several Finnish Health Care registries providing ecological validity and eliminating problems such as loss to follow-up. Although there are limitations to electronic patient records, such as being inconsistent and incomplete (Ougrin et al, 2021), the Finnish register has been shown to have high validity for register-based diagnoses of bipolar and psychotic disorders (Merikukka et al, 2018).
However, as noted by the authors, although the study employed a long follow-up period, this only extended until participants were 28 years old, which is prior to the age when risk of the onset of the disorders of interest is highest. As such, the findings likely represent an underestimation of the true risk for psychotic or bipolar disorders, which, if anything, adds weight to their argument for robust assessment at first presentation.
This paper highlights the strength of health care data linkage as an important resource for early identification and potential to delay or prevent the onset of mental health disorders.
Implications for practice
Improved treatment and formal assessment of young people who present to hospital with self-harm is needed given the serious psychiatric illnesses present in this population. The time from first self-harm presentation to diagnosis presents a critical window for intervention that must be capitalised on.
Proper assessment of young people presenting with self-harm rather than dismissal as a psychosocial crisis will lead to earlier intervention, more timely diagnosis and better outcomes (i.e. delay or even prevent the onset of illness and also reduce subsequent suicide risk). Therefore, healthcare services and systems need to be better equipped to detect and manage illness from the point of presentation to emergency departments through to ongoing care.
To date, peer-led aftercare services and safe spaces are increasing in popularity as a way of facilitating engagement in care after an emergency department presentation and as alternative interventions. These stand to make an important contribution, however, this research highlights the importance of ensuring that these are not implemented at the expense of clinical services and that blended models that combine peer support with clinical expertise are required.
Lastly, national registries are a useful resource for both service planning and research; they facilitate the tracking of people through the care system, allowing the accurate identification of high-risk populations and assessment of which clinical strategies work best and for whom.
Healthcare services and systems need to be better equipped to detect and manage illness from the point of presentation to emergency departments through to ongoing care.
Statement of interests
None declared.
Links
Primary paper
Bolhuis K, Lång U, Gyllenberg D, Kääriälä A, Veijola J, Gissler M, Kelleher I. (2021) Hospital Presentation for Self-Harm in Youth as a Risk Marker for Later Psychotic and Bipolar Disorders: A Cohort Study of 59 476 Finns. Schizophr Bull. 2021 May 15: sbab061. doi: 10.1093/schbul/sbab061. Epub ahead of print. PMID: 33991091.
Other references
Clements C, Jones S, Morriss R et al (2015) Self-harm in bipolar disorder: findings from a prospective clinical database. Journal of affective disorders 2015 173 113-119.
Forte A, Buscajoni A, Fiorillo A et al (2019) Suicidal risk following hospital discharge: a review. Harvard review of psychiatry 2019 27(4) 209-216.
Gillies D, Christou M. A, Dixon A. C, et al (2015) Prevalence and Characteristics of Self-Harm in Adolescents: Meta-Analyses of Community-Based Studies 1990-2015. J Am Acad Child Adolesc Psychiatry 2018 57(10) 733-741.
Haining K, Karagiorgou O, Gajwani R et al (2020). Prevalence and predictors of suicidality and non‐suicidal self‐harm among individuals at clinical high‐risk for psychosis: Results from a community‐recruited sample. Early intervention in psychiatry 2020
Kamal S, McGovern M, Kunideliene A et al (2021). A Comparison of Presentations with Self-Harm to Hospital in Lithuania and Ireland. International Journal of Environmental Research and Public Health 2021 18(5), 2418.
Kelleher I, Corcoran P, Keeley H et al (2013) Psychotic symptoms and population risk for suicide attempt: a prospective cohort study. JAMA psychiatry 2013 70(9) 940-948.
Merikukka M, Ristikari T, Tuulio-Henriksson A et al (2018) Childhood determinants for early psychiatric disability pension: a 10-year follow-up study of the 1987 Finnish Birth Cohort. International Journal of Social Psychiatry2018 64(8) 715-725.
Murphy J, Shevlin M, Hyland P et al (2018) Reconsidering the association between psychosis and suicide: a suicidal drive hypothesis. Psychosis 2018 10(4) 286-297.
National Institute for Health and Care Excellence (2013). Self-harm Quality Standard (QS34)
National Health and Medical Research Council (2009) NHMRC additional levels of evidence and grades for recommendations for developers of guidelines. Melbourne, Australia: NHMRC.
Olfson M, Marcus S. C, Bridge J. A. (2012) Emergency treatment of deliberate self-harm. Archives of General Psychiatry 2012 69(1) 80-88.
Ougrin D, Wong B. H. C, Vaezinejad M et al (2021) Pandemic-related emergency psychiatric presentations for self-harm of children and adolescents in 10 countries (PREP-kids): a retrospective international cohort study. European child & adolescent psychiatry 2021 1-13.
Paananen R, Gissler M. Cohort profile: the 1987 Finnish Birth Cohort. Int J Epidemiol 2012 41(4) 941-945.
Photo credits
- Photo by Annie Spratt on Unsplash
- Photo by Tiffany Tertipes on Unsplash
- Photo by Markus Winkler on Unsplash
