As a thought experiment: you see a 58 year-old male patient with no past psychiatric history, presenting to the emergency department by ambulance with signs and symptoms suggestive of a psychotic episode. The patient is triaged straight to liaison psychiatry. Notes from the paramedics record no current medication or relevant past medical history, no reported substance use, but they remark that the patient was “grabbing” at objects that weren’t visible and wonder if the patient is hallucinating. The patient’s symptoms include unusual thought content (largely around persecution by their neighbours, but it’s hard to pin down the detail because of significant thought disorganisation) and they deny hallucinations, but are witnessed in the department, alone, talking to themselves and laughing inappropriately. Engagement with cognitive testing is limited, but qualitatively, they have poor concentration and are disoriented in time and can only tell you they are “in a hospital”.
The patient’s presentation fits with a psychotic syndrome but the paramedics did describe behavior more consistent with visual than auditory hallucinations, the former being about half as common in psychosis, if you remember correctly, but sometimes visual and auditory hallucinations occur together (Clark et al., 2017).
Further, you reason that it’s unusual for orientation to be disturbed (you’re fairly sure the ICD-10 says that) and the epidemiology tells us the patient’s age is far above expected for a ‘classic’ first presentation of a primary psychotic disorder (onset is usually in late adolescence/early 20s; Buchanan and Carpenter, 2005). You can remember that brain atrophy is more common in older patients presenting with psychotic symptoms (Louhija et al, 2017) and also, there’s late-onset psychotic illness at around age 60 (Howard et al, 2000).
Do you send the patient for a magnetic resonance imaging (MRI) scan of their brain, concerned that there’s something “organic” driving their behaviour? It’ll cost the hospital between £100-200, take hours to get done and reported by a neuroradiologist and that’s assuming the patient will cooperate with this plan. Maybe it’s just better to treat the patient and worry about investigating later? MRIs are almost always normal anyway (well, probably almost always normal).
A new paper by Falkenberg et al (2017) investigates the clinical feasibility and utility of MRI in first episode psychosis (FEP), and helps answer these questions.

This new BJP study explores the feasibility and utility of performing an MRI scan in first episode psychosis.
Methods
Falkenberg et al (2017) recruited a research sample (RS; 106 FEPs and 98 controls) and a clinical sample (CS; 241 FEPs and 66 controls). They differed in the MRI protocol used, with the scans for the CS group being optimised for expert interpretation by a neuroradiologist (roughly, the images are of higher resolution), whereas the RS group were scanned using a protocol for research purposes (conversely, lower resolution). Additionally, the FEP patients in the research sample were recruited for (and their scans acquired and drawn from) the AESOP study (Morgan et al, 2006). The clinical sample FEP patients had scans acquired for clinical reasons, as part of a first clinical assessment with psychiatric services.
Neuroradiologists reviewed, interpreted and then described findings on all the MRI scans in both samples. The authors then reviewed reports, classifying each scan as abnormal or normal, further sub-classifying any abnormal findings (“lesions”) and the recommendation for follow-up (for example, if the lesion required the patient to be seen urgently, or routinely).
Results
Analyses presented in the paper include medication differences between the two samples; for example, patients in the RS were more likely to be on typical (older) antipsychotic medications, whereas patients in the CS were mostly taking atypical (newer) antipsychotic medication and had less lifetime medication exposure.
- One important finding was that in the clinical sample, patients had a statistically significant higher proportion of abnormal scans than the research sample (15.4% vs. 5.6%). Control participants in both groups were not significantly different.
- Perhaps most significantly, the recommendations for follow up (routine follow up or no follow up; the latter implying findings have no clinical significance) did not differ between either RS or CS groups.
- The types of abnormality found also differed, with cysts and asymmetry of the ventricles being most prevalent (1.9%) in the research group, whereas in the clinical group, white matter abnormalities (6%), cysts (2.6%) and 5.1% had cavum septi pellucidi (a ‘gap’ in the septum pellucidum, a structure towards the front of the brain that separates the ventricles and normally closes shortly after birth).
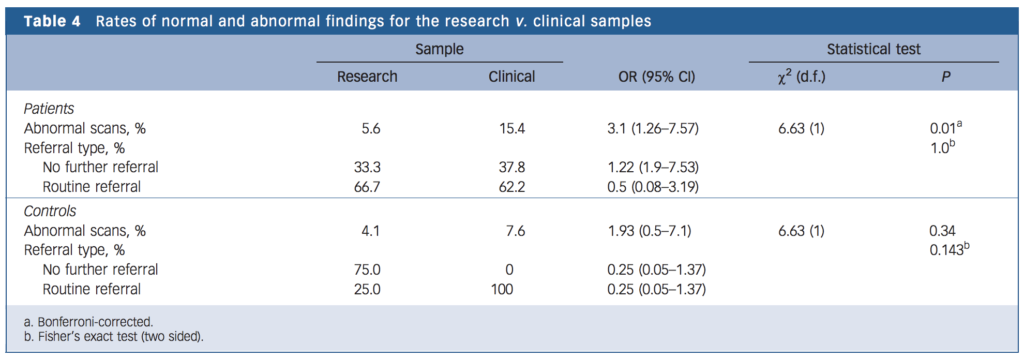
Radiological abnormalities were reported in 6% of the research sample and in 15% of the clinical sample, but none of the findings required a change in clinical management.
Limitations
Sample size and selection bias are acknowledged by the authors who declare that all participants came from roughly the same urban geographical area and their findings are consistent with other literature cited in the paper.
Implications for practice
The implications of Falkenberg’s paper are twofold:
- The first is that only 2.5% in the clinical sample couldn’t tolerate MRI. The scanner is often described as claustrophobic, noisy and to acquire high quality images, the patient is required to lay still for some time (around 30-40 minutes).
- The second is that (combined with the findings of other studies, e.g. Louhija et al, 2017) there is often pathology that contributes information that aids formulating the patient’s presentation and planning management. Traditionally, the clinical utility of neuroimaging has been viewed as “ruling out” the classical “organic” causes of psychotic syndromes. Indeed, a health-economic assessment (Albon et al, 2008) provides evidence for cost-efficacy if it is assumed that there is a 1% prevalence of MRI abnormality and assessment is completed between 1 and 3 months of presenting. Further, as early intervention services (in the UK) include patients aged up to 65 years, the need for robust evaluation of “organic” causes is even more relevant.
Returning to our hypothetical patient, neuroimaging is certainly indicated (alongside other tests); they have atypical demographics, atypical illness features and the list of differentials would certainly include the more classic “organic” causes including infection (e.g. viral encephalitis), neurodegenerative diseases (e.g. atypical or rarer dementias) and the immune system (e.g. autoimmune encephalitis). Some of these causes have catastrophic consequences if not detected and treated promptly. For this reason alone, there is an obvious utility for MRI to “rule out” treatable organic pathology.
Beyond these current clinical indications, there are considerations for advancing our understanding of the neurobiological basis of psychotic syndromes. Changes in the surface area of cortex (the ‘outer layer’ of the brain’s grey matter) appears to be a robust finding in MRI studies of schizophrenia (Yao et al, 2017) and while not definitive (i.e. this finding doesn’t clinch the diagnosis using only MRI scanning) such findings have potential as a future source of information that would weight clinical diagnosis toward or away from a primary psychotic disorder.
One limitation of current routine clinical MRI is that largely, it’s the structure of the brain that is imaged capturing abnormalities of the grey and white matter architecture. As evidence accumulates that the functioning of the brain differs in psychosis, newer imaging modalities (functional magnetic imaging, or fMRI) may have clinical use if robust protocols can be found that can be quickly and reliably acquired in clinical neuroimaging settings. Typically, fMRI is used for research where responses are elicited from stimuli presented to participants while measures (analogous to activity in the brain) are recorded by the scanner. One potential advance in this area is resting functional connectivity, where activity in the brain can be recorded while the patient does nothing during the scan (as for the familiar structural MRI) but these data are subjected to analyses that show how networks of brain regions behave (for an overview, see Hu et al 2017). Disruption to these networks may provide clues as to the nature of dysfunction in psychotic illnesses.

Life-threatening cases of psychosis with an ‘organic’ aetiology may be rare (e.g. brain tumours or encephalitis), but when the impact of missing them is so great, might it be worth assessing everyone?
Conflicts of interest
My research focuses on similar problems (identifying biomarkers of psychotic illness) using computer assisted- and automated techniques and given my biomedical focus, I am predisposed to be excited by results like these. I also work as a junior doctor in psychiatry (in the NHS), and am a member of the Royal College of Psychiatrists.
Links
Primary paper
Falkenberg I, Benetti S, Raffin M, Wuyts P, Pettersson-Yeo W, Dazzan P, Morgan KD, Murray RM, Reis Marques T, David AS, Jarosz J, Simmons A, Williams S, McGuire P. (2017) Clinical utility of magnetic resonance imaging in first-episode psychosis. Br J Psychiatry. 2017 May 4. pii: bjp.bp.116.195834. doi: 10.1192/bjp.bp.116.195834. [Epub ahead of print]
Other references
Clark, M.L. et al (2017) On the interconnectedness and prognostic value of visual and auditory hallucinations in first-episode psychosis. European Psychiatry, March, Volume 41, Pages 122–128, DOI: 10.1016/j.eurpsy.2016.10.011.
Louhija U.M., et al (2017) Brain atrophy is a frequent finding in elderly patients with first episode psychosis. International Psychogeriatrics. June, 1-5, DOI:10.1017/S1041610217000953
Buchanan R.W. and Carpenter W.T. (2005) Concept of schizophrenia. In Kaplan & Sadock’s Comprehensive Textbook of Psychiatry (8th edn) BJ Sadock & VA Sadock (Eds) Lippincott Williams & Wilkins.
Howard R, et al (2000). Late-onset schizophrenia and very-late-onset schizophrenia-like psychosis: an international consensus. American Journal of Psychiatry (157) pp. 172– 178.
Morgan, C. et al (2006) First episode psychosis and ethnicity: initial findings from the AESOP study. World Psychiatry. Feb; 5(1): pp. 40–46.
Albon E, et al (2008) Structural neuroimaging in psychosis: a systematic review and economic evaluation. Health Technology Assessement, Vol. 12(18). https://dx.doi.org/10.3310/hta12180
Yao, N, et al (2017) Inferring pathobiology from structural MRI in schizophrenia and bipolar disorder: Modeling head motion and neuroanatomical specificity. Human Brain Mapping, August, Vol 38(8) pp. 3757-3770. DOI: 10.1002/hbm.23612.
Hu, M-L et al (2017) A Review of the Functional and Anatomical Default Mode Network in Schizophrenia. Neuroscience Bulletin, February, 33(1), pp. 73–84. DOI 10.1007/s12264-016-0090-1
Photo credits
- See page for author [Public domain], via Wikimedia Commons

Hi
My daughters had 3 episodes of psychosis age 24. 28. 34
Every time admitted under mental health act.
had epilepsy as a child – settled on sodium valproate –
Every time she comes off aed – within a year psychosis occurs.
She gets put on antipsychotics
She’s only had 3 seizures in last 18 years –
Do you know of a neuropsychiatrist – we could get a second opinion from please.